Recognizing and Treating Peptic Ulcer Disease
Peptic ulcer disease (PUD) is one of the most common diseases affecting the gastroinestinal (GI) tract. Gastric ulcers, in the stomach, and duodenal ulcers, in the upper portion of the small intestine, occur most often.1 Under normal conditions, a physiologic balance occurs between gastric acid secretion and gastroduodenal mucosal defense.2 Because of mucosal injury, PUD occurs when the balance between the aggressive factors and the defensive mechanisms is disrupted or disturbed.2 PUD affects about 4.5 million individuals annually in the United States, and nearly 10% of the US population has evidence of a duodenal ulcer at some time.2 Additionally, the incidence of PUD has transitioned from predominance in men to comparable incidences in both men and women. The lifetime occurrence of PUD is about 11% to 14% in men and 8% to 11%, respectively.2
CAUSES/RISK FACTORS RELATING TO PUD
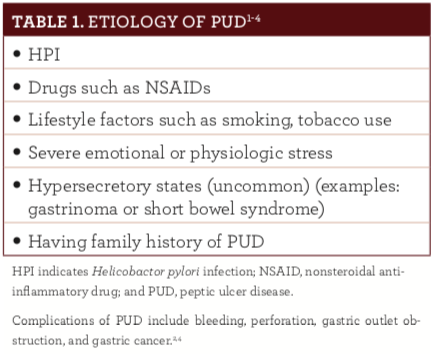
Most ulcers are caused by Helicobactor pylori infection (HPI) or nonsteriodal anti-inflammatory drug (NSAID) use. Both disrupt normal mucosal defense and repair, making the mucosa more susceptible to acid.2-5 HPI infection is common and also causes gastric cancer.3 The rate of HPI infection for duodenal ulcers in the United States is less than 75% for patients who do not use NSAIDs.2,4 Excluding pa- tients who used NSAIDs, 61% of duodenal ulcers and 63% of gastric ulcers were positive for HPI in one study.2 NSAIDs disturb the mucosal permeability barrier, making the mucosa susceptible to injury.2 Factors associated with a greater risk of duodenal ulcers with NSAID use include advanced age, a history of previous PUD, being female, concomitant use of anticoagulants, high combinations or doses of NSAIDs, long-term NSAID use, and severe comorbid illnesses.2,4 Older people are at greater risk of PUD because of high-risk medication use, including antiplatelet drugs, biophosphonates, selective serotonin reuptake inhibitors, and warfarin.4 Factors contributing to the etiology of PUD can be found in table 1.1-4
SIGNS AND SYMPTOMS
Symptoms for PUD depend on the location of the ulcer. Some patients may initially be asymptomatic.1 In general, those with PUD may present with episodic gnawing or burning epigastric pain, pain occurring 2 to 5 hours after meals or on an empty stomach, and nocturnal pain relieved by antacids, antisecretory agents, or food intake.2,4 A history of epigastric or episodic pain, relief of pain after food intake, and nighttime awakening because of pain, with relief following food intake, are the most specific findings for PUD and may aid in confirming a diagnosis.4 Less common features include heartburn, indigestion, intolerance of fatty foods, loss of appetite, a positive family history, and vomiting.4 The most important symptoms that ulcers cause are related to bleeding, according to the American College of Gastroenterology (ACG).1 Bleeding from an ulcer can be slow and go undetected or can cause life-threatening hemorrhage. Ulcers that bleed slowly may not produce symptoms until the individual becomes anemic. Symptoms of anemia include fatigue, pale skin color, and shortness of breath with exercise.1
TREATMENT OF PEPTIC ULCER DISEASE
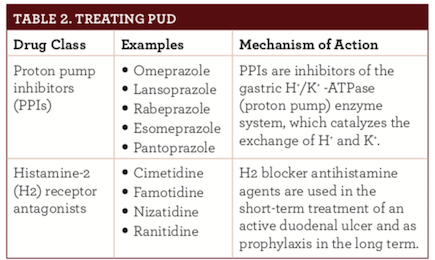
Treatment of PUD varies depending on the etiology and clinical presentation. The goals of pharmacotherapy are to eradicate HPI infection, to reduce morbidity, and to prevent complications in patients with PUD.1-4 Acid suppression is the general pharmacologic principle of medical management of acute bleeding from a peptic ulcer, using histamine-2 receptor antagonists and proton pump inhibitors (PPIs) (table 2).2
Gastroprotectant drugs have been developed for the protection of the mucosa, healing of mucosal damage, and stabilization of GI bleeding and are prescribed for the prevention of PUD, to promote healing, and as treatment for bleeding complications.5 Other agents used in PUD may include antimicrobials, bismuth subsalicylate, and cytoprotective agents, such as misoprostol and sucralfate.2
NSAIDs should be immediately discontinued in patients with positive HPI test results if clinically feasible, according to the ACG.2,3 For patients who must remain on NSAIDs, PPI maintenance is suggested to avert recurrences even after eradication of HPI.2,3
The 2017 ACG guidelines for the treatment of H pylori infection have reaffirmed testing for HPI before starting NSAID therapy. 3 The suggested primary therapy for HPI is PPI—based triple therapy. Antacids or a GI cocktail, classically an antacid with an anesthetic, such as viscous lidocaine and/or an antispasmodic, may be used as symptomatic therapy in the emergency department.2,3 Maintenance treatment with H2 blockers and/or PPIs for 1 year is indicated in high-risk patients.2,3
The ACG guidelines indicate that selection of an HPI management regimen should take into account previous antibiotic exposure(s). The ACG also includes the following therapeutic strategies for first- line treatment3:
- Ten to 14 days of bismuth quadruple therapy (bismuth, a PPI, tetracycline, and a nitroimidazole), especially in those with previous macrolide exposure or who are penicillin allergic (strong recommendation)
- Ten to 14 days of a concomitant PPI, clarithromycin, amoxicil- lin, and a nitroimidazole (strong recommendation)
- Fourteen days of clarithromycin triple therapy (clarithromycin, a PPI, and amoxicillin or metronidazole) should be reserved for patients with no previous history of macrolide exposure who live in regions where clarithromycin resistance among H pyloriisolates is known to be low (<15%)(conditional recommendation)
- Five to 7 days of sequential therapy with a PPI and amoxicillin, followed by 5 to 7 days with clarithromycin, a PPI, and a nitroimidazole (conditional recommendation)
- Seven days of a hybrid therapy with a PPI and amoxicillin, followed by 7 days with a PPI, amoxicillin, clarithromycin, and a nitroimidazole (conditional recommendation)
- Ten to 14 days of levofloxacin triple therapy (levofloxacin, a PPI, and amoxicillin)(conditional recommendation)
- Five to 7 days of fluoroquinolone sequential therapy (a PPI and amoxicillin), followed by 5 to 7 days of a PPI, fluoroquinolone, and nitroimidazol (conditional recommendation)
More information on the PUD guidelines can be found on the ACG website (gi.org/physician-resources/podcasts/the-american-journal-of-gastroenterology-author-podcasts/chey3/).
ROLE OF THE PHARMACIST
Pharmacists should be prepared to answer patients’ concerns and be familiar with the basics of PUD. They can screen for possible drug/ drug interactions and contraindications as well as counsel patients on the proper use of pharmacological agents used for the treatment of PUD, including adverse effects. Patients experiencing worsening symptoms should be directed to immediately seek medical care to prevent further complications.
Yvette C. Terrie, BSPharm, RPh is a consultant pharmacist and medical writer based in Haymarket, Virginia.
REFERENCES
1. Caufield SP, Schafer TW. Peptic ulcer disease. American Gastroenterological Asso- ciation website. patients.gi.org/topics/peptic-ulcer-disease/ Updated December 2012. Accessed May 25, 2018.
2. Anand BS. Peptic ulcer disease. Medscape website. emedicine.medscape.com/arti- cle/181753-overview. Updated January 29, 2017. Accessed May 25, 2018.
3. [Chey WD, Leontiadis GI, Howden CW, Moss SF. ACG clinical guideline: treat- ment of Helicobacter pylori infection. Am J Gastroenterol. 2017;112(2):212-239. doi: 10.1038/ajg.2016.563.
4. Fashner J, Gitu A. Diagnosis and treatment of peptic ulcer disease and H pyloriinfection. Am Fam Physician. 2015;91(4):236-242.
5. Scally B, Emberson JR, Spata E, et al. Effects of gastroprotectant drugs for the prevention and treatment of peptic ulcer disease and its complications: a meta-analysis of randomized trials. Lancet Gastroenterol Hepatol. 2018;3(4):231-241. doi: 10.1016/ S2468-1253(18)30037-2.

